Poliomyelitis, often called polio or infantile paralysis, is an infectious disease caused by the poliovirus. In about 0.5% of cases there is muscle weakness ...
Poliomyelitis
From Wikipedia, the free encyclopedia
"Polio" redirects here. For the virus, see
Poliovirus.
Not to be confused with
poliosis, a condition of the hair being or becoming white or grey.
, often called
polio or
infantile paralysis, is an
infectious disease caused by the
poliovirus. In about 0.5% of cases there is
muscle weakness resulting in an
inability to move.
[1] This can occur over a few hours to few days.
[1][2] The weakness most often involves the legs but may less commonly involve the muscles of the head, neck and
diaphragm. Many but not all people fully recover. In those with muscle weakness about 2% to 5% of children and 15% to 30% of adults die.
[1] Another 25% of people have minor symptoms such as fever and a sore throat and up to 5% have
headache, neck stiffness and pains in the arms and legs.
[1][2] These people are usually back to normal within one or two weeks. In up to 70% of infections
there are no symptoms.
[1] Years after recovery
post-polio syndrome may occur, with a slow development of muscle weakness similar to that which the person had during the initial infection.
[3]
Poliovirus is usually spread from person to person through
infected fecal matter entering the mouth.
[1] It may also be spread by food or water containing human feces and less commonly from infected
saliva.
[1][2]
Those who are infected may spread the disease for up to six weeks even
if no symptoms are present. The disease may be diagnosed by finding the
virus in the
feces or detecting
antibodies against it in the blood.
[1]
The disease is preventable with the
polio vaccine; however, a number of doses are required for it to be effective.
[2] The
United States Center for Disease Control recommends polio vaccination boosters for travelers and those who live in countries where the disease is occurring.
[4] Once infected there is no specific treatment.
[2] In 2013 polio affected 416 people down from 350,000 cases in 1988.
[2] In 2014 the disease was only spreading between people in
Afghanistan,
Nigeria, and
Pakistan.
[2] In 2015 Nigeria had stopped the spread of wild poliovirus.
[5]
Poliomyelitis has existed for thousands of years, with depictions of the disease in ancient art.
[1] The disease was first recognized as a distinct condition by
Michael Underwood in 1789
[1] and the virus that causes it was first identified in 1908 by
Karl Landsteiner.
[6] Major
outbreaks started to occur in the late 19th century in Europe and the United States.
[1] In the 20th century it became one of the most worrying
childhood diseases in these areas.
[7] The first polio vaccine was developed in the 1950s by
Jonas Salk.
[8] It is hoped that
vaccination efforts and early detection of cases will result in global
eradication of the disease by 2018.
[9] In 2013, however, there were reports of new cases in
Syria[10] and in May 2014, the
World Health Organization declared a
public health emergency of international concern due to outbreaks of the disease in Asia, Africa and the Middle East.
[11] The disease does not naturally occur in any other animals.
[1]
Signs and symptoms
Outcomes of poliovirus infection
| Outcome |
Proportion of cases[1] |
| No symptoms |
72% |
| Minor illness |
24% |
Nonparalytic aseptic
meningitis |
1–5% |
| Paralytic poliomyelitis |
0.1–0.5% |
| — Spinal polio |
79% of paralytic cases |
| — Bulbospinal polio |
19% of paralytic cases |
| — Bulbar polio |
2% of paralytic cases |
The term "poliomyelitis" is used to identify the disease caused by any of the three
serotypes of poliovirus. Two basic patterns of polio infection are described: a minor illness which does not involve the
central nervous system (CNS), sometimes called abortive poliomyelitis, and a major illness involving the CNS, which may be paralytic or nonparalytic.
[12] In most people with a
normal immune system, a poliovirus infection is
asymptomatic. Rarely, the infection produces minor symptoms; these may include upper
respiratory tract infection (
sore throat and fever),
gastrointestinal disturbances (nausea, vomiting,
abdominal pain, constipation or, rarely, diarrhea), and
influenza-like illness.
[1]
The virus enters the central nervous system in about 1% of infections. Most patients with CNS involvement develop nonparalytic
aseptic meningitis, with symptoms of headache, neck, back, abdominal and extremity pain, fever, vomiting,
lethargy, and irritability.
[13][14] About one to five in 1000 cases progress to
paralytic
disease, in which the muscles become weak, floppy and poorly
controlled, and, finally, completely paralyzed; this condition is known
as
acute flaccid paralysis.
[15] Depending on the site of paralysis, paralytic poliomyelitis is classified as spinal,
bulbar, or bulbospinal.
Encephalitis,
an infection of the brain tissue itself, can occur in rare cases, and
is usually restricted to infants. It is characterized by confusion,
changes in mental status, headaches, fever, and, less commonly,
seizures and
spastic paralysis.
[16]
Cause
Poliomyelitis is caused by infection with a member of the
genus Enterovirus known as
poliovirus (PV). This group of
RNA viruses colonize the
gastrointestinal tract[17] — specifically the
oropharynx and the
intestine. The incubation time (to the first signs and symptoms) ranges from three to 35 days, with a more common span of six to 20 days.
[1] PV
infects and causes disease in humans alone.
[18] Its
structure is very simple, composed of a single
(+) sense RNA genome enclosed in a protein shell called a
capsid.
[18]
In addition to protecting the virus’s genetic material, the capsid
proteins enable poliovirus to infect certain types of cells. Three
serotypes
of poliovirus have been identified—poliovirus type 1 (PV1), type 2
(PV2), and type 3 (PV3)—each with a slightly different capsid protein.
[19] All three are extremely
virulent and produce the same disease symptoms.
[18] PV1 is the most commonly encountered form, and the one most closely associated with paralysis.
[20]
Individuals who are exposed to the virus, either through infection or by
immunization with polio vaccine, develop
immunity. In immune individuals,
IgA antibodies against poliovirus are present in the
tonsils and gastrointestinal tract, and are able to block virus replication;
IgG and
IgM antibodies against PV can prevent the spread of the virus to motor neurons of the
central nervous system.
[21]
Infection or vaccination with one serotype of poliovirus does not
provide immunity against the other serotypes, and full immunity requires
exposure to each serotype.
[21]
A rare condition with a similar presentation, nonpoliovirus poliomyelitis, may result from infections with nonpoliovirus
enteroviruses.
[22]
Transmission
Poliomyelitis is highly contagious via the fecal-oral (intestinal source) and the oral-oral (oropharyngeal source) routes.
[21] In endemic areas, wild polioviruses can infect virtually the entire human population.
[23] It is seasonal in
temperate climates, with peak transmission occurring in summer and autumn.
[21] These seasonal differences are far less pronounced in
tropical areas.
[23] The time between first exposure and first symptoms, known as the
incubation period, is usually 6 to 20 days, with a maximum range of three to 35 days.
[24] Virus particles are excreted in the
feces for several weeks following initial infection.
[24] The disease is
transmitted primarily via the
fecal-oral route, by ingesting contaminated food or water. It is occasionally transmitted via the oral-oral route,
[20] a mode especially visible in areas with good sanitation and hygiene.
[21]
Polio is most infectious between seven and 10 days before and after the
appearance of symptoms, but transmission is possible as long as the
virus remains in the saliva or feces.
[20]
Factors that increase the risk of polio infection or affect the severity of the disease include
immune deficiency,
[25] malnutrition,
[26] physical activity immediately following the onset of paralysis,
[27] skeletal muscle injury due to
injection of vaccines or therapeutic agents,
[28] and
pregnancy.
[29] Although the virus can cross the
maternal-fetal barrier during pregnancy, the fetus does not appear to be affected by either maternal infection or polio vaccination.
[30] Maternal antibodies also cross the
placenta, providing
passive immunity that protects the infant from polio infection during the first few months of life.
[31]
As a precaution against infection, public
swimming pools were often closed in affected areas during poliomyelitis epidemics.
Pathophysiology
A blockage of the
lumbar anterior spinal cord
artery due to polio (PV3)
Poliovirus enters the body through the mouth, infecting the first cells with which it comes in contact — the
pharynx and
intestinal mucosa. It gains entry by binding to an
immunoglobulin-like receptor, known as the poliovirus receptor or
CD155, on the cell membrane.
[32] The virus then hijacks the
host cell's own machinery, and begins to
replicate. Poliovirus divides within gastrointestinal cells for about a week, from where it spreads to the
tonsils (specifically the
follicular dendritic cells residing within the tonsilar
germinal centers), the intestinal
lymphoid tissue including the
M cells of
Peyer's patches, and the deep
cervical and
mesenteric lymph nodes, where it multiplies abundantly. The virus is subsequently absorbed into the bloodstream.
[33]
Known as
viremia,
the presence of a virus in the bloodstream enables it to be widely
distributed throughout the body. Poliovirus can survive and multiply
within the blood and lymphatics for long periods of time, sometimes as
long as 17 weeks.
[34] In a small percentage of cases, it can spread and replicate in other sites, such as
brown fat, the
reticuloendothelial tissues, and muscle.
[35]
This sustained replication causes a major viremia, and leads to the
development of minor influenza-like symptoms. Rarely, this may progress
and the virus may invade the central nervous system, provoking a local
inflammatory response. In most cases, this causes a self-limiting inflammation of the
meninges, the layers of tissue surrounding the
brain, which is known as nonparalytic aseptic meningitis.
[13]
Penetration of the CNS provides no known benefit to the virus, and is
quite possibly an incidental deviation of a normal gastrointestinal
infection.
[36]
The mechanisms by which poliovirus spreads to the CNS are poorly
understood, but it appears to be primarily a chance event—largely
independent of the age, gender, or
socioeconomic position of the individual.
[36]
Paralytic polio
Denervation of
skeletal muscle tissue secondary to poliovirus infection can lead to paralysis.
In around 1% of infections, poliovirus spreads along certain nerve fiber pathways, preferentially replicating in and destroying
motor neurons within the
spinal cord,
brain stem, or
motor cortex.
This leads to the development of paralytic poliomyelitis, the various
forms of which (spinal, bulbar, and bulbospinal) vary only with the
amount of neuronal damage and inflammation that occurs, and the region
of the CNS affected.
The destruction of neuronal cells produces
lesions within the
spinal ganglia; these may also occur in the
reticular formation,
vestibular nuclei,
cerebellar vermis, and deep
cerebellar nuclei.
[36] Inflammation associated with
nerve cell destruction often alters the color and appearance of the gray matter in the
spinal column, causing it to appear reddish and swollen.
[13] Other destructive changes associated with paralytic disease occur in the
forebrain region, specifically the
hypothalamus and
thalamus.
[36] The molecular mechanisms by which poliovirus causes paralytic disease are poorly understood.
Early symptoms of paralytic polio include high fever, headache,
stiffness in the back and neck, asymmetrical weakness of various
muscles, sensitivity to touch,
difficulty swallowing,
muscle pain, loss of superficial and deep
reflexes,
paresthesia
(pins and needles), irritability, constipation, or difficulty
urinating. Paralysis generally develops one to ten days after early
symptoms begin, progresses for two to three days, and is usually
complete by the time the fever breaks.
[37]
The likelihood of developing paralytic polio increases with age, as
does the extent of paralysis. In children, nonparalytic meningitis is
the most likely consequence of CNS involvement, and paralysis occurs in
only one in 1000 cases. In adults, paralysis occurs in one in 75 cases.
[38] In children under five years of age, paralysis of one leg is most common; in adults, extensive paralysis of the
chest and
abdomen also affecting all four limbs—
quadriplegia—is more likely.
[39]
Paralysis rates also vary depending on the serotype of the infecting
poliovirus; the highest rates of paralysis (one in 200) are associated
with poliovirus type 1, the lowest rates (one in 2,000) are associated
with type 2.
[40]
Spinal polio
Spinal polio, the most common form of paralytic poliomyelitis, results from viral invasion of the motor neurons of the
anterior horn cells, or the
ventral (front)
grey matter section in the
spinal column, which are responsible for movement of the muscles, including those of the
trunk,
limbs, and the
intercostal muscles.
[15] Virus invasion causes inflammation of the nerve cells, leading to damage or destruction of motor neuron
ganglia. When spinal neurons die,
Wallerian degeneration takes place, leading to weakness of those muscles formerly
innervated by the now-dead neurons.
[41]
With the destruction of nerve cells, the muscles no longer receive
signals from the brain or spinal cord; without nerve stimulation, the
muscles
atrophy, becoming weak, floppy and poorly controlled, and finally completely paralyzed.
[15] Maximum paralysis progresses rapidly (two to four days), and usually involves fever and muscle pain. Deep
tendon reflexes are also affected, and are typically absent or diminished;
sensation (the ability to feel) in the paralyzed limbs, however, is not affected.
[42]
The extent of spinal paralysis depends on the region of the cord affected, which may be
cervical,
thoracic, or
lumbar.
[43] The virus may affect muscles on both sides of the body, but more often the paralysis is
asymmetrical.
[33] Any
limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms. Paralysis is often more severe
proximally (where the limb joins the body) than
distally (the
fingertips and
toes).
[33]
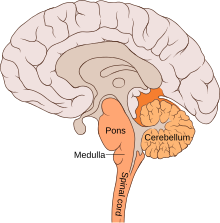
Bulbar polio
The location and anatomy of the bulbar region (in orange)
Making up about 2% of cases of paralytic polio, bulbar polio occurs when poliovirus invades and destroys nerves within the
bulbar region of the
brain stem.
[1] The bulbar region is a
white matter pathway that connects the
cerebral cortex to the brain stem. The destruction of these nerves weakens the muscles supplied by the
cranial nerves, producing symptoms of
encephalitis, and causes
difficulty breathing, speaking and swallowing.
[14] Critical nerves affected are the
glossopharyngeal nerve (which partially controls swallowing and functions in the throat, tongue movement, and taste), the
vagus nerve (which sends signals to the heart, intestines, and lungs), and the
accessory nerve (which controls upper neck movement). Due to the effect on swallowing, secretions of
mucus may build up in the airway, causing suffocation.
[37] Other signs and symptoms include
facial weakness (caused by destruction of the
trigeminal nerve and
facial nerve, which innervate the cheeks,
tear ducts, gums, and muscles of the face, among other structures),
double vision, difficulty in chewing, and abnormal
respiratory rate, depth, and rhythm (which may lead to
respiratory arrest).
Pulmonary edema and
shock are also possible and may be fatal.
[43]
Bulbospinal polio
Approximately 19% of all paralytic polio cases have both bulbar and
spinal symptoms; this subtype is called respiratory or bulbospinal
polio.
[1] Here, the virus affects the upper part of the cervical spinal cord (
cervical vertebrae C3 through C5), and paralysis of the
diaphragm occurs. The critical nerves affected are the
phrenic nerve (which drives the diaphragm to inflate the
lungs)
and those that drive the muscles needed for swallowing. By destroying
these nerves, this form of polio affects breathing, making it difficult
or impossible for the patient to breathe without the support of a
ventilator. It can lead to paralysis of the arms and legs and may also affect swallowing and heart functions.
[44]
Diagnosis
Paralytic poliomyelitis may be clinically suspected in individuals
experiencing acute onset of flaccid paralysis in one or more limbs with
decreased or absent tendon reflexes in the affected limbs that cannot be
attributed to another apparent cause, and without sensory or
cognitive loss.
[45]
A laboratory diagnosis is usually made based on recovery of poliovirus from a stool sample or a swab of the
pharynx.
Antibodies to poliovirus can be diagnostic, and are generally detected in the blood of infected patients early in the course of infection.
[1] Analysis of the patient's
cerebrospinal fluid (CSF), which is collected by a
lumbar puncture ("spinal tap"), reveals an increased number of
white blood cells (primarily
lymphocytes) and a mildly elevated protein level. Detection of virus in the CSF is diagnostic of paralytic polio, but rarely occurs.
[1]
If poliovirus is isolated from a patient experiencing acute flaccid paralysis, it is further tested through
oligonucleotide mapping (
genetic fingerprinting), or more recently by
PCR amplification, to determine whether it is "
wild type"
(that is, the virus encountered in nature) or "vaccine type" (derived
from a strain of poliovirus used to produce polio vaccine).
[46]
It is important to determine the source of the virus because for each
reported case of paralytic polio caused by wild poliovirus, an estimated
200 to 3,000 other contagious
asymptomatic carriers exist.
[47]
Prevention
Passive immunization
In 1950,
William Hammon at the
University of Pittsburgh purified the
gamma globulin component of the
blood plasma of polio survivors.
[48]
Hammon proposed the gamma globulin, which contained antibodies to
poliovirus, could be used to halt poliovirus infection, prevent disease,
and reduce the severity of disease in other patients who had contracted
polio. The results of a large
clinical trial
were promising; the gamma globulin was shown to be about 80% effective
in preventing the development of paralytic poliomyelitis.
[49] It was also shown to reduce the severity of the disease in patients who developed polio.
[48]
Due to the limited supply of blood plasma gamma globulin was later
deemed impractical for widespread use and the medical community focused
on the development of a polio vaccine.
[50]
Vaccine
Main article:
Polio vaccine
A child receiving an oral polio vaccine
Two types of vaccine are used throughout the world to combat polio.
Both types induce immunity to polio, efficiently blocking
person-to-person transmission of wild poliovirus, thereby protecting
both individual vaccine recipients and the wider community (so-called
herd immunity).
[51]
The first candidate
polio vaccine, based on one serotype of a live but
attenuated (weakened) virus, was developed by the
virologist Hilary Koprowski. Koprowski's prototype vaccine was given to an eight-year-old boy on 27 February 1950.
[52] Koprowski continued to work on the vaccine throughout the 1950s, leading to large-scale trials in the then
Belgian Congo and the vaccination of seven million children in Poland against serotypes PV1 and PV3 between 1958 and 1960.
[53]
The second inactivated virus vaccine was developed in 1952 by
Jonas Salk at the University of Pittsburgh, and announced to the world on 12 April 1955.
[54] The Salk vaccine, or inactivated poliovirus vaccine (IPV), is based on poliovirus grown in a type of monkey kidney
tissue culture (
vero cell line), which is chemically inactivated with
formalin.
[21] After two doses of IPV (given by
injection), 90% or more of individuals develop protective antibody to all three
serotypes of poliovirus, and at least 99% are immune to poliovirus following three doses.
[1]
Subsequently,
Albert Sabin
developed another live, oral polio vaccine (OPV). It was produced by
the repeated passage of the virus through nonhuman cells at sub
physiological temperatures.
[55]
The attenuated poliovirus in the Sabin vaccine replicates very
efficiently in the gut, the primary site of wild poliovirus infection
and replication, but the vaccine strain is unable to replicate
efficiently within
nervous system tissue.
[56]
A single dose of Sabin's oral polio vaccine produces immunity to all
three poliovirus serotypes in about 50% of recipients. Three doses of
live-attenuated OPV produce protective antibody to all three poliovirus
types in more than 95% of recipients.
[1] Human trials of Sabin's vaccine began in 1957,
[57]
and in 1958 it was selected, in competition with the live vaccines of
Koprowski and other researchers, by the US National Institutes of
Health.
[53] Licensed in 1962,
[57] it rapidly became the only polio vaccine used worldwide.
[53]
Because OPV is inexpensive, easy to administer, and produces
excellent immunity in the intestine (which helps prevent infection with
wild virus in areas where it is
endemic), it has been the vaccine of choice for controlling poliomyelitis in many countries.
[58]
On very rare occasions (about one case per 750,000 vaccine recipients),
the attenuated virus in OPV reverts into a form that can paralyze.
[24] Most
industrialized countries
have switched to IPV, which cannot revert, either as the sole vaccine
against poliomyelitis or in combination with oral polio vaccine.
[59]
Treatment
There is no
cure
for polio. The focus of modern treatment has been on providing relief
of symptoms, speeding recovery and preventing complications. Supportive
measures include
antibiotics to prevent infections in weakened muscles,
analgesics for pain, moderate exercise and a nutritious diet.
[60] Treatment of polio often requires long-term rehabilitation, including
occupational therapy,
physical therapy, braces, corrective shoes and, in some cases,
orthopedic surgery.
[43]
Portable
ventilators may be required to support breathing. Historically, a noninvasive, negative-pressure ventilator, more commonly called an
iron lung,
was used to artificially maintain respiration during an acute polio
infection until a person could breathe independently (generally about
one to two weeks). Today, many polio survivors with permanent
respiratory paralysis use modern
jacket-type negative-pressure ventilators worn over the chest and abdomen.
[61]
Other
historical treatments for polio include
hydrotherapy,
electrotherapy, massage and passive motion exercises, and surgical treatments, such as tendon lengthening and nerve grafting.
[15]
Prognosis
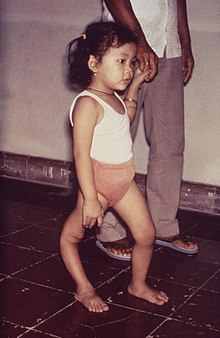
A child with a deformity of her right leg due to polio
Patients with abortive polio infections recover completely. In those
who develop only aseptic meningitis, the symptoms can be expected to
persist for two to ten days, followed by complete recovery.
[62]
In cases of spinal polio, if the affected nerve cells are completely
destroyed, paralysis will be permanent; cells that are not destroyed,
but lose function temporarily, may recover within four to six weeks
after onset.
[62]
Half the patients with spinal polio recover fully; one-quarter recover
with mild disability, and the remaining quarter are left with severe
disability.
[63] The degree of both acute paralysis and residual paralysis is likely to be proportional to the degree of
viremia, and
inversely proportional to the degree of
immunity.
[36] Spinal polio is rarely fatal.
[37]
Without respiratory support, consequences of poliomyelitis with
respiratory involvement include
suffocation or
pneumonia from aspiration of secretions.
[61] Overall, 5–10% of patients with paralytic polio die due to the paralysis of muscles used for breathing. The
case fatality rate (CFR) varies by age: 2–5% of children and up to 15–30% of adults die.
[1] Bulbar polio often causes death if respiratory support is not provided;
[44] with support, its CFR ranges from 25 to 75%, depending on the age of the patient.
[1][64] When intermittent positive pressure ventilation is available, the fatalities can be reduced to 15%.
[65]
Recovery
Many cases of poliomyelitis result in only temporary paralysis.
[15] Nerve impulses return to the formerly paralyzed muscle within a month, and recovery is usually complete in six to eight months.
[62] The
neurophysiological
processes involved in recovery following acute paralytic poliomyelitis
are quite effective; muscles are able to retain normal strength even if
half the original motor neurons have been lost.
[66]
Paralysis remaining after one year is likely to be permanent, although
modest recoveries of muscle strength are possible 12 to 18 months after
infection.
[62]
One mechanism involved in recovery is nerve terminal sprouting, in
which remaining brainstem and spinal cord motor neurons develop new
branches, or axonal sprouts.
[67] These sprouts can
reinnervate orphaned muscle fibers that have been denervated by acute polio infection,
[68] restoring the fibers' capacity to contract and improving strength.
[69]
Terminal sprouting may generate a few significantly enlarged motor
neurons doing work previously performed by as many as four or five
units:
[38]
a single motor neuron that once controlled 200 muscle cells might
control 800 to 1000 cells. Other mechanisms that occur during the
rehabilitation phase, and contribute to muscle strength restoration,
include
myofiber hypertrophy—enlargement of muscle fibers through exercise and activity—and transformation of
type II muscle fibers to
type I muscle fibers.
[68][70]
In addition to these physiological processes, the body possesses a
number of compensatory mechanisms to maintain function in the presence
of residual paralysis. These include the use of weaker muscles at a
higher than usual intensity relative to the
muscle's maximal capacity, enhancing athletic development of previously little-used muscles, and using
ligaments for stability, which enables greater mobility.
[70]
Complications
Residual complications of paralytic polio often occur following the initial recovery process.
[14] Muscle
paresis and paralysis can sometimes result in
skeletal
deformities, tightening of the joints and movement disability. Once the
muscles in the limb become flaccid, they may interfere with the
function of other muscles. A typical manifestation of this problem is
equinus foot (similar to
club foot).
This deformity develops when the muscles that pull the toes downward
are working, but those that pull it upward are not, and the foot
naturally tends to drop toward the ground. If the problem is left
untreated, the
Achilles tendons
at the back of the foot retract and the foot cannot take on a normal
position. Polio victims that develop equinus foot cannot walk properly
because they cannot put their heel on the ground. A similar situation
can develop if the arms become paralyzed.
[71]
In some cases the growth of an affected leg is slowed by polio, while
the other leg continues to grow normally. The result is that one leg is
shorter than the other and the person limps and leans to one side, in
turn leading to deformities of the spine (such as
scoliosis).
[71] Osteoporosis and increased likelihood of
bone fractures may occur. An intervention to prevent or lessen length disparity can be to perform an
epiphysiodesis on the distal femoral and proximal tibial/fibular condyles, so that limb's growth is artificially stunted, and by the time of
epiphyseal (growth) plate
closure, the legs are more equal in length. Alternatively, a person can
be fitted with custom made footwear which corrects the difference in
leg lengths. Other surgery to re-balance muscular agonist/antagonist
imbalances may also be helpful. Extended use of braces or wheelchairs
may cause compression
neuropathy, as well as a loss of proper function of the
veins in the legs, due to pooling of blood in paralyzed lower limbs.
[44][72] Complications from prolonged immobility involving the
lungs,
kidneys and
heart include
pulmonary edema,
aspiration pneumonia,
urinary tract infections,
kidney stones,
paralytic ileus,
myocarditis and
cor pulmonale.
[44][72]
Post-polio syndrome
Between 25% and 50% of individuals who have recovered from paralytic
polio in childhood can develop additional symptoms decades after
recovering from the acute infection,
[73] notably new muscle weakness and extreme fatigue. This condition is known as
post-polio syndrome (PPS) or post-polio sequelae.
[74] The symptoms of PPS are thought to involve a failure of the over-sized
motor units created during the recovery phase of the paralytic disease.
[75][76]
Contributing factors that increase the risk of PPS include aging with
loss of neuron units, the presence of a permanent residual impairment
after recovery from the acute illness, and both overuse and disuse of
neurons. PPS is a slow, progressive disease, and there is no specific
treatment for it.
[74] Post-polio syndrome is not an infectious process, and persons experiencing the syndrome do not shed poliovirus.
[1]
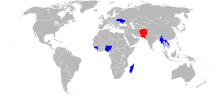
Epidemiology
|
Reported polio cases in 2015[77]
|
|
|
| Country |
Wild
cases |
Circulating
vaccine-
derived
cases |
Transmission
status |
 Pakistan Pakistan |
52 |
2 |
endemic |
 Afghanistan Afghanistan |
19 |
0 |
endemic |
 Madagascar Madagascar |
0 |
10 |
circulating vaccine-
derived only |
 Laos Laos |
0 |
6 |
circulating vaccine-
derived only |
 Guinea Guinea |
0 |
4 |
circulating vaccine-
derived only |
 Myanmar Myanmar |
0 |
2 |
circulating vaccine-
derived only |
 Ukraine Ukraine |
0 |
2 |
circulating vaccine-
derived only |
 Nigeria Nigeria |
0 |
1 |
circulating vaccine-
derived only |
| Total |
71 |
27 |
Following the widespread use of poliovirus vaccine in the mid-1950s,
the incidence of poliomyelitis declined dramatically in many
industrialized countries. A global effort to
eradicate polio began in 1988, led by the
World Health Organization,
UNICEF, and
The Rotary Foundation.
[78]
These efforts have reduced the number of annual diagnosed cases by
99.9%; from an estimated 350,000 cases in 1988 to a low of 483 cases in
2001, after which it remained at a level of about 1,000 - 2000 cases per
year for a number of years.
[79][80] In 2015, cases decreased to 98.
[77][81] Polio is one of only two diseases currently the subject of a global
eradication program, the other being
Guinea worm disease.
[82] So far, the only diseases completely eradicated by humankind are
smallpox, declared so, in 1980,
[83][84] and
rinderpest, likewise, in 2011.
[85] A number of eradication milestones have already been reached, and several regions of the world have been certified polio-free.
A concern is the presence of circulating vaccine-derived polioviruses
(cVDPV). The OPV is not perfect: while the genetic characteristics are
carefully balanced to maximize efficacy and minimize virulence, it is
possible for the OPV to mutate. As a result, persons given the OPV can
acquire acute or chronic infections; or can transmit (circulate) mutated
OPV to other people. It is likely that cVDPV cases will exceed wild
cases in the near future, making it desirable to discontinue use of the
OPV as soon as safely possible.
[86]
Emergency declaration
In April 2012, the World Health Assembly declared the completion of
polio eradication a programmatic emergency for global public health.
[87]
Americas
The
Americas were declared polio-free in 1994.
[88]
Western Pacific
In 2000 polio was declared to have been officially eliminated in 37 Western Pacific countries, including China and Australia.
[89][90]
Despite eradication ten years prior, an outbreak was confirmed in
China in September 2011 involving a strain prevalent in neighboring
Pakistan.
[91]
Europe
Europe was declared polio-free in 2002.
[92] On 1 September, 2015 WHO confirmed 2 cases of circulating vaccine-derived poliovirus type 1 in Ukraine.
[93]
South-East Asia
The last case of polio in the region was in India in January 2011.
[94]
Since January 2011, there have been no reported cases of the wild polio
infections in India, and in February 2012 the country was taken off the
WHO list of polio endemic countries. It was reported that if there are
no cases of wild polio in the country for two more years, it would be
declared as a polio-free country.
[95][96]
On March 27, 2014 the WHO announced the eradication of poliomyelitis
in the South-East Asia Region, which includes eleven countries:
Bangladesh,
Bhutan,
North Korea,
India,
Indonesia,
Maldives,
Myanmar,
Nepal,
Sri Lanka,
Thailand and
Timor-Leste.
[97] With the addition of this region, 80 per cent of the world population lives in polio-free regions.
[97]
Syria
In 2015, polio was believed to remain
endemic in only two countries:
Pakistan, and
Afghanistan,
[97][98][99][100] although it continued to cause epidemics in other nearby countries due to hidden or reestablished transmission.
[101]
In
Syria difficulties in executing immunization programs in the ongoing
civil war led to a return of polio, probably in 2012,
[102] acknowledged by the WHO in 2013.
[103][104] 15 cases were confirmed among children in
Syria between October and November 2013 in
Deir Ezzor. Later, two more cases, each one in rural
Damascus and
Aleppo,
were identified. It was the first outbreak in Syria since 1999. Doctors
and international public health agencies report more than 90 cases of
polio in Syria, with fears of contagion in rebel areas from lack of
sanitation and safe-water services.
[105] In May 2014, the World Health Organization declared polio's renewed spread a
world health emergency.
[106][107]
A vaccination campaign in Syria operated literally under fire and lead to the deaths of several vaccinators,
[108] but returned vaccination coverage to pre-war levels.
[109] No new cases have been reported since January 2014; vaccination continues, and Iraq is also being closely monitored.
[110][111]
Africa
In 2003 in
northern Nigeria—a country which at that time was considered provisionally polio free—a
fatwa was issued declaring that the polio vaccine was designed to render children sterile.
[112]
Subsequently, polio reappeared in Nigeria and spread from there to
several other countries. In 2013, nine health workers administering
polio vaccine were targeted and killed by gunmen on motorcycles in
Kano, but this was the first
[113] and last attack.
[114] Local traditional and religious leaders and polio survivors worked to revive the campaign,
[115]
and Nigeria has not had a polio case since July 24, 2014. In September
2015, Nigeria is removed from polio-endemic list. If no new cases
appear, it will be declared polio-free in 2017.
[116]
In 2013 the Center for Disease Control received reports of 183 cases of polio in
Somalia, 14 in
Kenya and 8 cases in the
Somali Region of Ethiopia,
[117] but Africa had no confirmed cases of wild poliovirus (WPV) in 2015.
[98] A case of circulating vaccine-derived poliovirus (cVDPV) type 2 was detected in
Siguiri in
Guinea's
Kankan region, in August 2014.
[118] In September 2015, a case of cVDPV in Mali was confirmed by the WHO.
[118]
Afghanistan and Pakistan
This is the last remaining region with wild polio cases. Both major sides of the Afghan civil war support polio vaccination
[119] and polio rates are declining rapidly in Afghanistan, with only 19 cases in 2015.
[98][115]
In
Pakistan there were 53 cases in 2015, the highest number for any country.
[98][115] Vaccination in Pakistan is hindered by conflict and organizational problems. The militant
Pakistani Taliban claims vaccination is a Western plot to
sterilise local children.
[120] 66 vaccinators were killed in 2013 and 2014.
[121][122] Cases have dropped by 70% in 2015; reasons include Dh440 million support from the
United Arab Emirates to vaccinate more than ten million children,
[122][123] changes in the military situation, and arrests of some of those who attacked polio workers.
[120][124]
History
The effects of polio have been known since
prehistory;
Egyptian paintings and carvings depict otherwise healthy people with withered limbs, and children walking with canes at a young age.
[125] The first clinical description was provided by the English physician
Michael Underwood in 1789, where he refers to polio as "a debility of the lower extremities".
[126] The work of physicians
Jakob Heine in 1840 and
Karl Oskar Medin in 1890 led to it being known as
Heine–Medin disease.
[127] The disease was later called
infantile paralysis, based on its propensity to affect children.
Before the 20th century, polio infections were rarely seen in infants
before six months of age, most cases occurring in children six months
to four years of age. Poorer
sanitation of the time resulted in a constant exposure to the virus, which enhanced a natural
immunity
within the population. In developed countries during the late 19th and
early 20th centuries, improvements were made in community sanitation,
including better
sewage
disposal and clean water supplies. These changes drastically increased
the proportion of children and adults at risk of paralytic polio
infection, by reducing childhood exposure and immunity to the disease.
[128]
Small localized paralytic polio
epidemics began to appear in Europe and the United States around 1900.
[129] Outbreaks reached
pandemic
proportions in Europe, North America, Australia, and New Zealand during
the first half of the 20th century. By 1950 the peak age incidence of
paralytic poliomyelitis in the United States had shifted from infants to
children aged five to nine years, when the risk of paralysis is
greater; about one-third of the cases were reported in persons over 15
years of age.
[130] Accordingly, the rate of paralysis and death due to polio infection also increased during this time.
[129]
In the United States, the 1952 polio epidemic became the worst outbreak
in the nation's history. Of nearly 58,000 cases reported that year
3,145 died and 21,269 were left with mild to disabling paralysis.
[131] Intensive care medicine has its origin in the fight against polio.
[132] Most hospitals in the 1950s had limited access to
iron lungs
for patients unable to breathe without mechanical assistance.
Respiratory centers designed to assist the most severe polio patients,
first established in 1952 at the Blegdam Hospital of
Copenhagen by
Danish anesthesiologist Bjørn Ibsen, were the harbingers of subsequent
intensive care units (ICU). (A year later, Ibsen would establish the world's first dedicated ICU.)
[133]
The polio epidemics not only altered the lives of those who survived them, but also brought profound cultural changes, spurring
grassroots fund-raising campaigns that would revolutionize medical
philanthropy, and giving rise to the modern field of
rehabilitation therapy. As one of the largest disabled groups in the world, polio survivors also helped to advance the modern
disability rights movement through campaigns for the social and civil rights of the
disabled. The World Health Organization estimates that there are 10 to 20 million polio survivors worldwide.
[134] In 1977 there were 254,000 persons living in the United States who had been paralyzed by polio.
[135]
According to doctors and local polio support groups, some 40,000 polio
survivors with varying degrees of paralysis live in Germany, 30,000 in
Japan, 24,000 in France, 16,000 in Australia, 12,000 in Canada and
12,000 in the United Kingdom.
[134] Many
notable individuals have survived polio
and often credit the prolonged immobility and residual paralysis
associated with polio as a driving force in their lives and careers.
[136]
The disease was very well publicized during the polio epidemics of
the 1950s, with extensive media coverage of any scientific advancements
that might lead to a cure. Thus, the scientists working on polio became
some of the most famous of the century. Fifteen scientists and two
laymen who made important contributions to the knowledge and treatment
of poliomyelitis are honored by the
Polio Hall of Fame, which was dedicated in 1957 at the
Roosevelt Warm Springs Institute for Rehabilitation in
Warm Springs, Georgia,
US. In 2008 four organizations (Rotary International, the World Health
Organization, the U.S. Centers for Disease Control and UNICEF) were
added to the Hall of Fame.
[137][138]
World Polio Day (24 October) was established by
Rotary International to commemorate the birth of
Jonas Salk,
who led the first team to develop a vaccine against poliomyelitis. Use
of this inactivated poliovirus vaccine and subsequent widespread use of
the oral poliovirus vaccine developed by
Albert Sabin
led to establishment of the Global Polio Eradication Initiative (GPEI)
in 1988. Since then, GPEI has reduced polio worldwide by 99%.
[139]
Etymology
The term derives from the
Ancient Greek poliós (
πολιός), meaning "grey",
myelós (
µυελός “marrow”), referring to the grey matter of the
spinal cord, and the suffix
-itis, which denotes
inflammation.,
[13]
i.e., inflammation of the spinal cord’s grey matter, although a severe
infection can extend into the brainstem and even higher structures,
resulting in
polioencephalitis, producing a
lack of ability to breathe that requires mechanical assistance such as an
iron lung.
Society and culture
References
 A man with a small right leg due to poliomyelitis
A man with a small right leg due to poliomyelitis Pakistan
Pakistan Afghanistan
Afghanistan Madagascar
Madagascar Laos
Laos Guinea
Guinea Myanmar
Myanmar Ukraine
Ukraine Nigeria
Nigeria





No comments:
Post a Comment