Dec 30, 2013 · Dengue fever and dengue hemorrhagic fever (DHF) are viral diseases transmitted by Aedes mosquitoes, usually Aedes Aegypti. The four dengue viruses (DEN-1 ...
Dengue fever
From Wikipedia, the free encyclopedia
Dengue fever (
UK // or
US //), also known as
breakbone fever, is a
mosquito-borne tropical disease caused by the
dengue virus. Symptoms include
fever,
headache,
muscle and
joint pains, and a characteristic
skin rash that is
similar to measles. In a small proportion of cases, the disease develops into the life-threatening
dengue hemorrhagic fever, resulting in
bleeding,
low levels of blood platelets and blood plasma leakage, or into
dengue shock syndrome, where
dangerously low blood pressure occurs.
Dengue is transmitted by several species of
mosquito within the
genus Aedes, principally
A. aegypti. The virus has five different types;
[1] infection with one type usually gives lifelong
immunity
to that type, but only short-term immunity to the others. Subsequent
infection with a different type increases the risk of severe
complications. As there is no commercially available
vaccine, prevention is sought by reducing the habitat and the number of mosquitoes and limiting exposure to bites.
Treatment of acute dengue is supportive, using either oral or intravenous
rehydration for mild or moderate disease, and
intravenous fluids and
blood transfusion
for more severe cases. The number of cases of dengue fever has
increased dramatically since the 1960s, with between 50 and 528 million
people infected yearly.
[2][3]
Early descriptions of the condition date from 1779, and its viral cause
and transmission were understood by the early 20th century. Dengue has
become a global problem since the
Second World War and is
endemic
in more than 110 countries. Apart from eliminating the mosquitoes, work
is ongoing on a vaccine, as well as medication targeted directly at the
virus.
Signs and symptoms
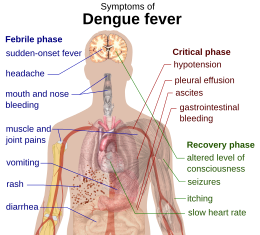
Schematic depiction of the symptoms of dengue fever
Typically, people infected with dengue virus are
asymptomatic (80%) or only have mild symptoms such as an uncomplicated fever.
[2][4][5] Others have more severe illness (5%), and in a small proportion it is life-threatening.
[2][5] The
incubation period (time between exposure and onset of symptoms) ranges from 3 to 14 days, but most often it is 4 to 7 days.
[6]
Therefore, travelers returning from endemic areas are unlikely to have
dengue if fever or other symptoms start more than 14 days after arriving
home.
[7] Children often experience symptoms similar to those of the
common cold and
gastroenteritis (vomiting and diarrhea)
[8] and have a greater risk of severe complications,
[7][9] though initial symptoms are generally mild but include high fever.
[9]
Clinical course
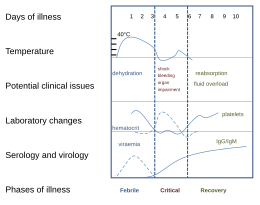
Clinical course of dengue fever
[10]
The characteristic symptoms of dengue are sudden-onset fever,
headache (typically located behind the eyes), muscle and joint pains,
and a rash. The alternative name for dengue, "breakbone fever", comes
from the associated muscle and joint pains.
[2][11] The course of infection is divided into three phases: febrile, critical, and recovery.
[10]
The febrile phase involves high fever, potentially over 40 °C
(104 °F), and is associated with generalized pain and a headache; this
usually lasts two to seven days.
[10][11] Nausea and vomiting may also occur.
[9] A rash occurs in 50–80% of those with symptoms
[11][12] in the first or second day of symptoms as
flushed skin, or later in the course of illness (days 4–7), as a
measles-like rash.
[12][13] A rash described as "islands of white in a sea of red" has also been observed.
[14] Some
petechiae (small red spots that do not disappear when the skin is pressed, which are caused by broken
capillaries) can appear at this point,
[10] as may some mild bleeding from the
mucous membranes of the mouth and nose.
[7][11] The fever itself is classically
biphasic or saddleback in nature, breaking and then returning for one or two days.
[13][14]
The rash of dengue fever in the acute stage of the infection
blanches when pressed
In some people, the disease proceeds to a critical phase as fever resolves.
[9] During this period there is leakage of plasma from the blood vessels which typically lasts one to two days.
[10] This may result in fluid accumulation in the
chest and
abdominal cavity as well as
depletion of fluid from the circulation and
decreased blood supply to vital organs.
[10] There may also be organ dysfunction and severe
bleeding, typically from the
gastrointestinal tract.
[7][10] Shock (dengue shock syndrome) and hemorrhage (dengue hemorrhagic fever) occur in less than 5% of all cases of dengue,
[7] however those who have previously been infected with other
serotypes of dengue virus ("secondary infection") are at an increased risk.
[7][15] This critical phase, while rare, occurs relatively more commonly in children and young adults.
[9]
The rash that commonly forms during the recovery from dengue fever with its classic islands of white in a sea of red.
The recovery phase occurs next, with resorption of the leaked fluid into the bloodstream.
[10] This usually lasts two to three days.
[7] The improvement is often striking, and can be accompanied with severe
itching and a
slow heart rate.
[7][10] Another rash may occur with either a
maculopapular or a
vasculitic appearance, which is followed by peeling of the skin.
[9] During this stage, a
fluid overload state may occur; if it
affects the brain, it may cause a
reduced level of consciousness or
seizures.
[7] A feeling of
fatigue may last for weeks in adults.
[9]
Associated problems
Dengue can occasionally affect several other
body systems,
[10] either in isolation or along with the classic dengue symptoms.
[8] A decreased level of consciousness occurs in 0.5–6% of severe cases, which is attributable either to
inflammation of the brain by the virus or indirectly as a result of impairment of vital organs, for example, the
liver.
[8][14][16]
Other neurological disorders have been reported in the context of dengue, such as
transverse myelitis and
Guillain-Barré syndrome.
[8][16] Infection of the heart and
acute liver failure are among the rarer complications.
[7][10]
Cause
Virology
Main article:
Dengue virus
Dengue fever virus (DENV) is an
RNA virus of the family
Flaviviridae; genus
Flavivirus. Other members of the same genus include
yellow fever virus,
West Nile virus,
St. Louis encephalitis virus,
Japanese encephalitis virus,
tick-borne encephalitis virus,
Kyasanur forest disease virus, and
Omsk hemorrhagic fever virus.
[14] Most are transmitted by
arthropods (mosquitoes or
ticks), and are therefore also referred to as
arboviruses (
arthropod-
borne viruses).
[14]
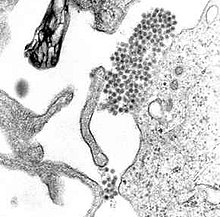
The dengue virus
genome (genetic material) contains about 11,000
nucleotide bases, which
code for the three different types of protein molecules (C, prM and E) that form the
virus particle
and seven other types of protein molecules (NS1, NS2a, NS2b, NS3, NS4a,
NS4b, NS5) that are only found in infected host cells and are required
for replication of the virus.
[15][17] There are five
[1] strains of the virus, called
serotypes, of which the first four are referred to as DENV-1, DENV-2, DENV-3 and DENV-4.
[4] The fifth type was announced in 2013.
[1] The distinctions between the serotypes are based on their
antigenicity.
[18]
Transmission
Dengue virus is primarily transmitted by
Aedes mosquitoes, particularly
A. aegypti.
[4] These mosquitoes usually live between the
latitudes of 35° North and 35° South below an
elevation of 1,000 metres (3,300 ft).
[4] They typically bite during the day, particularly in the early morning and in the evening,
[19][20] but they are able to bite and thus spread infection at any time of day all during the year.
[21] Other
Aedes species that transmit the disease include
A. albopictus,
A. polynesiensis and
A. scutellaris.
[4] Humans are the primary
host of the virus,
[4][14] but it also circulates in nonhuman
primates.
[22] An infection can be acquired via a single bite.
[23]
A female mosquito that takes a blood meal from a person infected with
dengue fever, during the initial 2–10 day febrile period, becomes itself
infected with the virus in the cells lining its gut.
[24] About 8–10 days later, the virus spreads to other tissues including the mosquito's
salivary glands
and is subsequently released into its saliva. The virus seems to have
no detrimental effect on the mosquito, which remains infected for life.
[6] Aedes aegypti
is particularly involved, as it prefers to lay its eggs in artificial
water containers, to live in close proximity to humans, and to feed on
people rather than other
vertebrates.
[6]
Dengue can also be transmitted via infected
blood products and through
organ donation.
[25][26] In countries such as
Singapore, where dengue is endemic, the risk is estimated to be between 1.6 and 6 per 10,000
transfusions.
[27] Vertical transmission (from mother to child) during pregnancy or at birth has been reported.
[28] Other person-to-person modes of transmission have also been reported, but are very unusual.
[11]
The genetic variation in dengue viruses is region specific, suggestive
that establishment into new territories is relatively infrequent,
despite dengue emerging in new regions in recent decades.
[9]
Predisposition
Severe disease is more common in babies and young children, and in
contrast to many other infections it is more common in children that are
relatively well nourished.
[7] Other
risk factors for severe disease include female sex, high
body mass index,
[9] and
viral load.
[29] While each serotype can cause the full spectrum of disease,
[15] virus strain is a risk factor.
[9]
Infection with one serotype is thought to produce lifelong immunity to
that type, but only short-term protection against the other three.
[4][11]
The risk of severe disease from secondary infection increases if
someone previously exposed to serotype DENV-1 contracts serotype DENV-2
or DENV-3, or if someone previously exposed to DENV-3 acquires DENV-2.
[17] Dengue can be life-threatening in people with
chronic diseases such as
diabetes and
asthma.
[17]
Polymorphisms (normal variations) in particular
genes
have been linked with an increased risk of severe dengue complications.
Examples include the genes coding for the proteins known as
TNFα,
mannan-binding lectin,
[2] CTLA4,
TGFβ,
[15] DC-SIGN,
PLCE1, and particular
forms of
human leukocyte antigen from gene variations of
HLA-B.
[9][17] A common genetic abnormality, especially in Africans, known as
glucose-6-phosphate dehydrogenase deficiency, appears to increase the risk.
[29] Polymorphisms in the genes for the
vitamin D receptor and
FcγR seem to offer protection against severe disease in secondary dengue infection.
[17]
Mechanism
When a mosquito carrying dengue virus bites a person, the virus
enters the skin together with the mosquito's saliva. It binds to and
enters
white blood cells,
and reproduces inside the cells while they move throughout the body.
The white blood cells respond by producing a number of signaling
proteins, such as
cytokines and
interferons,
which are responsible for many of the symptoms, such as the fever, the
flu-like symptoms and the severe pains. In severe infection, the virus
production inside the body is greatly increased, and many more organs
(such as the
liver and the
bone marrow) can be affected. Fluid from the bloodstream leaks through the wall of small blood vessels into body cavities due to
capillary permeability.
As a result, less blood circulates in the blood vessels, and the blood
pressure becomes so low that it cannot supply sufficient blood to vital
organs. Furthermore, dysfunction of the bone marrow due to infection of
the
stromal cells
leads to reduced numbers of platelets, which are necessary for
effective blood clotting; this increases the risk of bleeding, the other
major complication of dengue fever.
[29]
Viral replication
Once inside the skin, dengue virus binds to
Langerhans cells (a population of
dendritic cells in the skin that identifies pathogens).
[29] The virus
enters the cells through binding between viral proteins and
membrane proteins on the Langerhans cell, specifically the
C-type lectins called DC-SIGN,
mannose receptor and
CLEC5A.
[15] DC-SIGN, a non-specific receptor for foreign material on dendritic cells, seems to be the main point of entry.
[17] The dendritic cell moves to the nearest
lymph node. Meanwhile, the virus genome is translated in membrane-bound vesicles on the cell's
endoplasmic reticulum,
where the cell's protein synthesis apparatus produces new viral
proteins that replicate the viral RNA and begin to form viral particles.
Immature virus particles are transported to the
Golgi apparatus, the part of the cell where some of the proteins receive necessary sugar chains (
glycoproteins). The now mature new viruses bud on the surface of the infected cell and are released by
exocytosis. They are then able to enter other white blood cells, such as
monocytes and
macrophages.
[15]
The initial reaction of infected cells is to produce interferon, a
cytokine that raises a number of defenses against viral infection through the
innate immune system by augmenting the production of a large group of proteins mediated by the
JAK-STAT pathway. Some serotypes of dengue virus appear to have mechanisms to slow down this process. Interferon also activates the
adaptive immune system, which leads to the generation of
antibodies against the virus as well as
T cells that directly attack any cell infected with the virus.
[15] Various antibodies are generated; some bind closely to the viral proteins and target them for
phagocytosis (ingestion by
specialized cells
and destruction), but some bind the virus less well and appear instead
to deliver the virus into a part of the phagocytes where it is not
destroyed but is able to replicate further.
[15]
Severe disease
It is not entirely clear why secondary infection with a different
strain of dengue virus places people at risk of dengue hemorrhagic fever
and dengue shock syndrome. The most widely accepted hypothesis is that
of
antibody-dependent enhancement
(ADE). The exact mechanism behind ADE is unclear. It may be caused by
poor binding of non-neutralizing antibodies and delivery into the wrong
compartment of white blood cells that have ingested the virus for
destruction.
[15][17] There is a suspicion that ADE is not the only mechanism underlying severe dengue-related complications,
[2][16] and various lines of research have implied a role for T cells and soluble factors such as cytokines and the
complement system.
[29]
Severe disease is marked by the problems of capillary permeability
(an allowance of fluid and protein normally contained within blood to
pass) and disordered
blood clotting.
[8][9] These changes appear associated with a disordered state of the endothelial
glycocalyx, which acts as a
molecular filter of blood components.
[9] Leaky capillaries (and the critical phase) are thought to be caused by an immune system response.
[9] Other processes of interest include infected cells that become
necrotic—which affect both coagulation and
fibrinolysis (the opposing systems of blood clotting and clot degradation)—and low platelets in the blood, also a factor in normal clotting.
[29]
Diagnosis
|
|
| Worsening abdominal pain |
| Ongoing vomiting |
| Liver enlargement |
| Mucosal bleeding |
| High hematocrit with low platelets |
| Lethargy or restlessness |
| Serosal effusions |
The diagnosis of dengue is typically made clinically, on the basis of reported symptoms and
physical examination; this applies especially in endemic areas.
[2] However, early disease can be difficult to differentiate from other
viral infections.
[7] A probable diagnosis is based on the findings of fever plus two of the following:
nausea and vomiting, rash, generalized pains,
low white blood cell count, positive
tourniquet test, or any warning sign (see table) in someone who lives in an
endemic area.
[30] Warning signs typically occur before the onset of severe dengue.
[10]
The tourniquet test, which is particularly useful in settings where no
laboratory investigations are readily available, involves the
application of a
blood pressure cuff at between the
diastolic and systolic pressure for five minutes, followed by the counting of any
petechial hemorrhages; a higher number makes a diagnosis of dengue more likely with the cut off being more than 10 to 20 per 1 inch
2 (6.25 cm
2).
[10][31]
The diagnosis should be considered in anyone who develops a fever within two weeks of being in the
tropics or
subtropics.
[9] It can be difficult to distinguish dengue fever and
chikungunya, a similar viral infection that shares many symptoms and occurs in similar parts of the world to dengue.
[11] Often, investigations are performed to exclude other conditions that cause similar symptoms, such as
malaria,
leptospirosis,
viral hemorrhagic fever,
typhoid fever,
meningococcal disease,
measles, and
influenza.
[7][32]
The earliest change detectable on laboratory investigations is a low white blood cell count, which may then be followed by
low platelets and
metabolic acidosis.
[7] A moderately elevated level of
aminotransferase (
AST and
ALT) from the liver is commonly associated with low platelets and white blood cells.
[9] In severe disease, plasma leakage results in
hemoconcentration (as indicated by a rising
hematocrit) and
hypoalbuminemia.
[7] Pleural effusions or
ascites can be detected by physical examination when large,
[7] but the demonstration of fluid on
ultrasound may assist in the early identification of dengue shock syndrome.
[2][7] The use of ultrasound is limited by lack of availability in many settings.
[2] Dengue shock syndrome is present if
pulse pressure drops to ≤ 20 mm Hg along with peripheral vascular collapse.
[9] Peripheral vascular collapse is determined in children via delayed
capillary refill, rapid heart rate, or cold extremities.
[10]
While warning signs are an important aspect for early detection of
potential serious disease, the evidence for any specific clinical or
laboratory marker is weak.
[33]
Classification
The
World Health Organization's 2009 classification divides dengue fever into two groups: uncomplicated and severe.
[2][30]
This replaces the 1997 WHO classification, which needed to be
simplified as it had been found to be too restrictive, though the older
classification is still widely used
[30] including by the World Health Organization's Regional Office for South-East Asia as of 2011.
[34]
Severe dengue is defined as that associated with severe bleeding,
severe organ dysfunction, or severe plasma leakage while all other cases
are uncomplicated.
[30] The 1997 classification divided dengue into undifferentiated fever, dengue fever, and dengue hemorrhagic fever.
[7][35]
Dengue hemorrhagic fever was subdivided further into grades I–IV. Grade
I is the presence only of easy bruising or a positive tourniquet test
in someone with fever, grade II is the presence of spontaneous bleeding
into the skin and elsewhere, grade III is the clinical evidence of
shock, and grade IV is shock so severe that blood pressure and
pulse cannot be detected.
[35] Grades III and IV are referred to as "dengue shock syndrome".
[30][35]
Laboratory tests
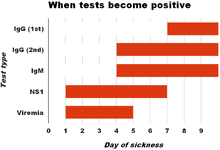
Graph of when laboratory tests for dengue fever become positive. Day
zero refers to the start of symptoms, 1st refers to in those with a
primary infection, and 2nd refers to in those with a secondary
infection.
[9]
The diagnosis of dengue fever may be confirmed by microbiological laboratory testing.
[30][36] This can be done by virus isolation in
cell cultures,
nucleic acid detection by
PCR, viral
antigen detection (such as for
NS1) or specific
antibodies (serology).
[17][32]
Virus isolation and nucleic acid detection are more accurate than
antigen detection, but these tests are not widely available due to their
greater cost.
[32] Detection of NS1 during the febrile phase of a primary infection may be greater than 90%
sensitive however is only 60–80% in subsequent infections.
[9] All tests may be negative in the early stages of the disease.
[7][17] PCR and viral antigen detection are more accurate in the first seven days.
[9]
In 2012 a PCR test was introduced that can run on equipment used to
diagnose influenza; this is likely to improve access to PCR-based
diagnosis.
[37]
These laboratory tests are only of diagnostic value during the acute
phase of the illness with the exception of serology. Tests for dengue
virus-specific antibodies, types
IgG and
IgM,
can be useful in confirming a diagnosis in the later stages of the
infection. Both IgG and IgM are produced after 5–7 days. The highest
levels (
titres)
of IgM are detected following a primary infection, but IgM is also
produced in reinfection. IgM becomes undetectable 30–90 days after a
primary infection, but earlier following re-infections. IgG, by
contrast, remains detectable for over 60 years and, in the absence of
symptoms, is a useful indicator of past infection. After a primary
infection IgG reaches peak levels in the blood after 14–21 days. In
subsequent re-infections, levels peak earlier and the titres are usually
higher. Both IgG and IgM provide protective immunity to the infecting
serotype of the virus.
[6][11][17]
In testing for IgG and IgM antibodies there may be cross-reactivity
with other flaviviruses which may result in a false positive after
recent infections or vaccinations with yellow fever virus or Japanese
encephalitis.
[9]
The detection of IgG alone is not considered diagnostic unless blood
samples are collected 14 days apart and a greater than fourfold increase
in levels of specific IgG is detected. In a person with symptoms, the
detection of IgM is considered diagnostic.
[6]
Prevention
A 1920s photograph of efforts to disperse standing water and thus decrease mosquito populations
There are no approved
vaccines for the dengue virus.
[2] Prevention thus depends on control of and protection from the bites of the mosquito that transmits it.
[19][38] The World Health Organization recommends an Integrated Vector Control program consisting of five elements:
[19]
- Advocacy, social mobilization and legislation to ensure that public health bodies and communities are strengthened;
- Collaboration between the health and other sectors (public and private);
- An integrated approach to disease control to maximize use of resources;
- Evidence-based decision making to ensure any interventions are targeted appropriately; and
- Capacity-building to ensure an adequate response to the local situation.
The primary method of controlling
A. aegypti is by eliminating its
habitats.
[19] This is done by getting rid of open sources of water, or if this is not possible, by adding
insecticides or
biological control agents to these areas.
[19] Generalized spraying with
organophosphate or
pyrethroid insecticides, while sometimes done, is not thought to be effective.
[5]
Reducing open collections of water through environmental modification
is the preferred method of control, given the concerns of negative
health effects from insecticides and greater logistical difficulties
with control agents.
[19] People can prevent mosquito bites by wearing clothing that fully covers the skin, using
mosquito netting while resting, and/or the application of
insect repellent (
DEET being the most effective).
[23]
However, these methods appear not to be sufficiently effective, as the
frequency of outbreaks appears to be increasing in some areas, probably
due to urbanization increasing the habitat of
A. aegypti. The range of the disease appears to be expanding possibly due to climate change.
[1]
Anti-dengue day
International Anti-Dengue Day is observed every year on June 15th.
[39] The idea was first agreed upon in 2010 with the first event held in
Jakarta,
Indonesia in 2011.
[39] Further events were held in 2012 in
Yangon,
Myanmar and in 2013 in
Vietnam.
[39]
Goals are to increase public awareness about dengue, mobilize resources
for its prevention and control and, to demonstrate the Asian region’s
commitment in tackling the disease.
[40]
Management
There are no specific
antiviral drugs for dengue, however maintaining proper fluid balance is important.
[9] Treatment depends on the symptoms.
[41]
Those who are able to drink, are passing urine, have no "warning signs"
and are otherwise healthy can be managed at home with daily follow up
and
oral rehydration therapy.
[41]
Those who have other health problems, have "warning signs" or who
cannot manage regular follow up should be cared for in hospital.
[7][41] In those with severe dengue care should be provided in an area where there is access to an
intensive care unit.
[41]
Intravenous hydration, if required, is typically only needed for one or two days.
[41] The rate of fluid administration is titrated to a
urinary output of 0.5–1 mL/kg/h, stable
vital signs and normalization of hematocrit.
[7] The smallest amount of fluid required to achieve this is recommended.
[41] Invasive medical procedures such as
nasogastric intubation,
intramuscular injections and arterial punctures are avoided, in view of the bleeding risk.
[7] Paracetamol (acetaminophen) is used for fever and discomfort while
NSAIDs such as
ibuprofen and
aspirin are avoided as they might aggravate the risk of bleeding.
[41] Blood transfusion is initiated early in people presenting with unstable vital signs in the face of a
decreasing hematocrit, rather than waiting for the hemoglobin concentration to decrease to some predetermined "transfusion trigger" level.
[42] Packed red blood cells or
whole blood are recommended, while
platelets and
fresh frozen plasma are usually not.
[42] There is not enough evidence to determine if
corticosteroids have a positive or negative effect in dengue fever.
[43]
During the recovery phase intravenous fluids are discontinued to prevent a state of
fluid overload.
[7] If fluid overload occurs and vital signs are stable, stopping further fluid may be all that is needed.
[42] If a person is outside of the critical phase, a
loop diuretic such as
furosemide may be used to eliminate excess fluid from the circulation.
[42]
Epidemiology
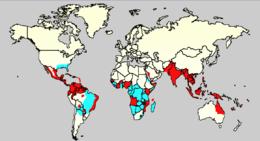
Dengue distribution in 2006
Epidemic dengue and A. aegypti
A. aegypti, without epidemic dengue
Most people with dengue recover without any ongoing problems.
[30] The fatality rate is 1–5%,
[7] and less than 1% with adequate treatment;
[30] however those who develop significantly low blood pressure may have a fatality rate of up to 26%.
[7] Dengue is
common in more than 110 countries.
[7] It infects 50 to 528 million people worldwide a year, leading to half a million hospitalizations,
[2][3] and approximately 25,000 deaths.
[8]
For the decade of the 2000s, 12 countries in Southeast Asia were
estimated to have about 3 million infections and 6,000 deaths annually.
[44] It is reported in at least 22 countries in Africa; but is likely present in all of them with 20% of the population at risk.
[45] This makes it one of the most common
vector-borne diseases worldwide.
[33]
Infections are most commonly acquired in the urban environment.
[6]
In recent decades, the expansion of villages, towns and cities in the
areas in which it is common, and the increased mobility of people has
increased the number of epidemics and circulating viruses. Dengue fever,
which was once confined to Southeast Asia, has now spread to Southern
China, countries in the Pacific Ocean and America,
[6] and might pose a threat to Europe.
[5]
Rates of dengue increased 30 fold between 1960 and 2010.
[46] This increase is believed to be due to a combination of urbanization, population growth, increased international travel, and
global warming.
[2]
The geographical distribution is around the equator. Of the 2.5 billion
people living in areas where it is common 70% are from Asia and the
Pacific.
[46]
An infection with dengue is second only to malaria as a diagnosed cause
of fever among travelers returning from the developing world.
[11] It is the most common viral disease transmitted by arthropods,
[15] and has a
disease burden estimated at 1,600
disability-adjusted life years per million population.
[17] The World Health Organization counts dengue as one of seventeen
neglected tropical diseases.
[47]
Like most arboviruses, dengue virus is maintained in nature in cycles
that involve preferred blood-sucking vectors and vertebrate hosts.
[6] The viruses are maintained in the forests of Southeast Asia and Africa by transmission from female
Aedes mosquitoes—of species other than
A. aegypti—to their offspring and to lower primates.
[6] In towns and cities, the virus is primarily transmitted by the highly domesticated
A. aegypti. In rural settings the virus is transmitted to humans by
A. aegypti and other species of
Aedes such as
A. albopictus.
[6] Both these species had expanding ranges in the second half of the 20th century.
[9]
In all settings the infected lower primates or humans greatly increase
the number of circulating dengue viruses, in a process called
amplification.
[6]
History
The first record of a case of probable dengue fever is in a Chinese medical encyclopedia from the
Jin Dynasty (265–420 AD) which referred to a "water poison" associated with flying insects.
[48][49] The primary vector,
A. aegypti, spread out of Africa in the 15th to 19th centuries due in part to increased globalization secondary to the
slave trade.
[9]
There have been descriptions of epidemics in the 17th century, but the
most plausible early reports of dengue epidemics are from 1779 and 1780,
when an epidemic swept across Asia, Africa and North America.
[49] From that time until 1940, epidemics were infrequent.
[49]
In 1906, transmission by the
Aedes mosquitoes was confirmed,
and in 1907 dengue was the second disease (after yellow fever) that was
shown to be caused by a virus.
[50] Further investigations by
John Burton Cleland and
Joseph Franklin Siler completed the basic understanding of dengue transmission.
[50]
The marked spread of dengue during and after the
Second World War
has been attributed to ecologic disruption. The same trends also led to
the spread of different serotypes of the disease to new areas, and to
the emergence of dengue hemorrhagic fever. This severe form of the
disease was first reported in the
Philippines in 1953; by the 1970s, it had become a major cause of
child mortality and had emerged in the Pacific and the Americas.
[49]
Dengue hemorrhagic fever and dengue shock syndrome were first noted in
Central and South America in 1981, as DENV-2 was contracted by people
who had previously been infected with DENV-1 several years earlier.
[14]
Etymology
The origins of the Spanish word
dengue are not certain, but it is possibly derived from
dinga in the
Swahili phrase
Ka-dinga pepo, which describes the disease as being caused by an
evil spirit.
[48] Slaves in the West Indies having contracted dengue were said to have the posture and gait of a
dandy, and the disease was known as "dandy fever".
[51][52]
The term "break-bone fever" was applied by physician and
United States Founding Father Benjamin Rush, in a 1789 report of the 1780 epidemic in
Philadelphia. In the report title he uses the more formal term "bilious remitting fever".
[53] The term dengue fever came into general use only after 1828.
[52] Other historical terms include "breakheart fever" and "la dengue".
[52]
Terms for severe disease include "infectious thrombocytopenic purpura"
and "Philippine", "Thai", or "Singapore hemorrhagic fever".
[52]
Research
Research efforts to prevent and treat dengue include various means of vector control,
[54] vaccine development, and antiviral drugs.
[38]
With regards to vector control, a number of novel methods have been
used to reduce mosquito numbers with some success including the
placement of the guppy (
Poecilia reticulata) or
copepods in standing water to eat the mosquito larvae.
[54] Attempts are ongoing to infect the mosquito population with bacteria of the
Wolbachia genus, which makes the mosquitoes partially resistant to dengue virus.
[9][55] There are also trials with genetically modified male
A. aegypti that after release into the wild mate with females, and render their offspring unable to fly.
[56]
There are ongoing programs working on a dengue vaccine to cover all four serotypes.
[38] Now that there is a fifth serotype this will need to be factored in.
[1] One of the concerns is that a vaccine could increase the risk of severe disease through
antibody-dependent enhancement (ADE).
[57]
The ideal vaccine is safe, effective after one or two injections,
covers all serotypes, does not contribute to ADE, is easily transported
and stored, and is both affordable and cost-effective.
[57] As of 2012, a number of vaccines were undergoing testing.
[20][57] The most developed is based on a weakened combination of the yellow fever virus and each of the four dengue serotypes.
[20][58] Two studies of a vaccine found it was 60% effective and prevented more than 80 to 90% of severe cases.
[59][60] It is hoped that the first products will be commercially available by 2015.
[38]
Apart from attempts to control the spread of the
Aedes mosquito and work to develop a vaccine against dengue, there are ongoing efforts to develop
antiviral drugs that would be used to treat attacks of dengue fever and prevent severe complications.
[61][62] Discovery of the structure of the viral proteins may aid the development of effective drugs.
[62] There are several plausible targets. The first approach is inhibition of the viral
RNA-dependent RNA polymerase (coded by NS5), which copies the viral genetic material, with
nucleoside analogs. Secondly, it may be possible to develop specific
inhibitors of the viral
protease (coded by NS3), which
splices viral proteins.
[63] Finally, it may be possible to develop
entry inhibitors, which stop the virus entering cells, or inhibitors of the
5′ capping process, which is required for viral replication.
[61]
Notes






No comments:
Post a Comment