I have never forgotten this idea. But, it went against me during my colonoscopy because they gave me too much and I was hallucinating when I woke up and couldn't walk without help and had to be wheelchaired out to my car and have my wife drive me home.
HOwever, the first time I was mostly conscious and this was much better for me because that level of anesthesia allowed me to witness on the TV of them going up into my colon and wasn't painful because I could even tell them when it was uncomfortable. So, next time (a few years from now when I do this I won't want the full anesthesia because it feels like I'm still recovering from all that in some ways by eliminating all the toxins of the anesthesia from my body. When I woke up spiritually something was very wrong and I knew this. So, this really wasn't okay with me until about 6 hours later when I was able to keep down and not throw up my heart medicine and thyroid medicine. So, next time I will ask for a minimum anesthesia so I'm basically awake for the colonoscopy.
But, if you are having an endoscopy it is better to be under. I though (thinking macho) that I could handle it on low anesthesia but choking on an endoscope as it goes down into your stomach is not fun at all because of your gag reflex. So, this can get a little painful and even with anesthesia the only real pain I had for a week was a sore throat from the endoscopy.
The best part of all this is being on Medicare when you do this because basically it's sort of free at this point except for your monthly payment to Medicare which is nominal compared to the full cost of a colonoscopy at a hospital.
begin quote from:
https://en.wikipedia.org/wiki/Colorectal_polyp
A colorectal polyp is a polyp (fleshy growth) occurring on the lining of the colon or
rectum. Untreated colorectal polyps can develop into colorectal cancer.Colorectal polyp
From Wikipedia, the free encyclopedia
| Colon polyps | |
|---|---|
 |
|
| Polyp of sigmoid colon as revealed by colonoscopy. Approximately 1 cm in diameter. The polyp was removed by snare cautery | |
| Classification and external resources | |
| Specialty | gastroenterology |
| ICD-10 | K63.5 & various |
| MedlinePlus | 000266 |
| eMedicine | med/414 |
| MeSH | C23.300.825 |
Gross appearance of a colectomy specimen containing two colorectal polyps and one invasive colorectal carcinoma
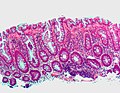
Micrograph of a tubular adenoma, the most common type of dysplastic polyp in the colon.
Micrograph of a tubular adenoma – dysplastic epithelium (dark purple) on left of image; normal epithelium (blue) on right. H&E stain.
Micrograph of a villous adenoma. These polyps are considered to have a high risk of malignant transformation. H&E stain.
Colorectal polyps are often classified by their behaviour (i.e. benign vs. malignant) and/or etiology (e.g. as a consequence of inflammatory bowel disease). They may be benign (e.g. hyperplastic polyp), pre-malignant (e.g. tubular adenoma) or malignant (e.g. colorectal adenocarcinoma).
Contents
Types
The most common general classification is:- hyperplastic,
- neoplastic (adenomatous & malignant),
- hamartomatous and,
- inflammatory.
Hyperplastic polyp
Most hyperplastic polyps are found in the distal colon and rectum.[3] They have no malignant potential,[3] which means that they are no more likely than normal tissue to eventually become a cancer.Hyperplastic polyps are serrated polyps. Hyperplastic polyps have three histologic patterns of growth: microvesicular, goblet cell and mucin poor.
Hyperplastic polyposis syndrome is a rare condition that has been defined by the World Health Organization as either:
-
- Five or more hyperplastic polyps proximal to the sigmoid colon, with two polyps greater than 10mm in diameter; or
- Any number of hyperplastic polyps proximal to the sigmoid colon in a person with a first degree relative who has hyperplastic polyposis syndrome; or
- More than 30 hyperplastic polyps of any size throughout the colon and rectum.[4]
Neoplastic polyp
A neoplasm is a tissue whose cells have lost its normal differentiation. They can be either benign growths or malignant growths. The malignant growths can either have primary or secondary causes.Adenomas
Neoplastic polyps of the bowel are often benign hence called adenomas. An adenoma is tumor glandular tissue, that has not (yet) gained the properties of a cancer.The common adenomas of the colon (colorectal adenoma) are the tubular, tubulovillous, villous, and sessile serrated (SSA).[3]
As is evident from their name, sessile serrated and traditional serrated adenomas (TSAs) have a serrated appearance and can be difficult to distinguish microscopically from hyperplastic polyps.[3] Making this distinction is important, however, since SSAs and TSAs have the potential to become cancers,[4] while hyperplastic polyps do not.[3]
The villous subdivision are associated with the highest malignant potential because they generally have the largest surface area. (This is because the villi are projections into the lumen and hence have a bigger surface area.) However, villous adenomas are no more likely than tubular or tubulovillous adenomas to become cancerous if their sizes are all the same.[3]
Hamartomatous polyp
They are growths, like tumours found in organs as a result of faulty development. They are normally made up of a mixture of tissues. They contain mucus-filled glands, with retention cysts, abundant connective tissue, and a chronic cellular infiltration of eosinophils.[5] They grow at the normal rate of the host tissue and rarely cause problems such as compression. A common example of a hamartomatous lesion is a strawberry naevus. Hamartomatous polyps are often found by chance; occurring in syndromes such as Peutz-Jegher Syndrome or Juvenile Polyposis Syndrome.Peutz-Jeghers syndrome is associated with polyps of the GI tract and also increased pigmentation around the lips, genitalia, buccal mucosa feet and hands. People are often diagnosed with Peutz-Jegher after presenting at around the age of 9 with an intussusception. The polyps themselves carry little malignant potential but because of potential coexisting adenomas there is a 15% chance of colonic malignancy.
Juvenile polyps are hamartomatous polyps which often become evident before twenty years of age, but can also be seen in adults. They are usually solitary polyps found in the rectum which most commonly present with rectal bleeding. Juvenile polyposis syndrome is characterised by the presence of more than five polyps in the colon or rectum, or numerous juvenile polyps throughout the gastrointestinal tract, or any number of juvenile polyps in any person with a family history of juvenile polyposis. People with juvenile polyposis have an increased risk of colon cancer.[4]
Inflammatory polyp
These are polyps which are associated with inflammatory conditions such as Ulcerative Colitis and Crohns disease.Symptoms
Colorectal polyps are not usually associated with symptoms.[2] When they occur, symptoms include rectal bleeding, bloody stools, abdominal pain and fatigue.[2] A change in bowel habits may occur including constipation and diarrhoea.[6] Occasionally, if a polyp is big enough to cause a bowel obstruction, there may be nausea, vomiting and severe constipation.[6]Screening and diagnosis
Colorectal polyps can be detected using a faecal occult blood test, flexible sigmoidoscopy, colonoscopy, virtual colonoscopy, digital rectal examination, barium enema or a pill camera.[6]When does a polyp become a problem?
Malignant potential is associated with- degree of dysplasia
- Type of polyp (e.g. villous adenoma):
- Tubular Adenoma: 5% risk of cancer
- Tubulovillous adenoma: 20% risk of cancer
- Villous adenoma: 40% risk of cancer
- Size of polyp:
- <1 cancer="" class="noprint Inline-Template Template-Fact" cm="<1%" nbsp="" of="" risk="" style="white-space: nowrap;" sup="">[citation needed]
Prevention
Diet and lifestyle are believed to play a large role in whether colorectal polyps form. Studies show there to be a protective link between consumption of cooked green vegetables, brown rice, legumes, and dried fruit and decreased incidence of colorectal polyps.[7]Treatment
Polyps can be removed during a colonoscopy or sigmoidoscopy using a wire loop that cuts the stalk of the polyp and cauterises it to prevent bleeding.[6] Many "defiant" polyps—large, flat, and otherwise laterally spreading adenomas—may be removed endoscopically by a technique called endoscopic mucosal resection (EMR), which involves injection of fluid underneath the lesion to lift it and thus facilitate surgical excision. These techniques may be employed as an alternative to a much-more-invasive colectomy.[8]Structure
Polyps are either pedunculated (attached to the intestinal wall by a stalk) or sessile (grow directly from the wall).[9]See also
Additional images
-
Microvesicular hyperplastic polyp. H&E stain.
References
- Classen, Meinhard; G. N. J. Tytgat; Charles J. Lightdale (2002). Gastroenterological Endoscopy. Thieme. p. 303. ISBN 1-58890-013-4.
External links
- "How I Do It" — Removing large or sessile colonic polyps. Dr. Brian Saunders MD FRCP; St. Mark’s Academic Institute; Harrow, Middlesex, UK. Retrieved April 9, 2008.
- Villous Adenoma - Medscape
- http://www.netdoctor.co.uk/diseases/facts/colonpolyps.htm
- http://www.clevelandclinic.org/registries/inherited/jp.htm
- Adenomas (serrated, tubular, tubulovillous, villous) and hyperplastic polyps
- Case of Tubulovillous Adenoma
- Tubulovillous adenoma, Colon
- Polyps explanation and risks








No comments:
Post a Comment